Inside the app that’s bridging faith and mental health in Boston’s Black communities
Author: Madelaine Millar
Date: 02.09.24
Numerous studies have found that Black Americans are more likely to experience severe depression than their white counterparts, and less likely to receive a diagnosis or treatment. In fact, the research concluded that Black people are less likely to receive adequate treatment for a wide variety of health issues — and Khoury College’s Teresa O’Leary believes tech can help to address that gap.
O’Leary was recently awarded her doctorate in personal health informatics after crafting an app-based mental health intervention for Black church community members who experienced depression, or who supported a loved one with depression. The intervention was part of a larger project called Smart and Connected Churches, in which multidisciplinary researchers from Khoury College, the Bouvé College of Health Sciences, Boston Medical Center, and Georgia Tech worked with members of Boston-area Black churches — the project’s intended user base — to design a health intervention app called ChurchConnect.
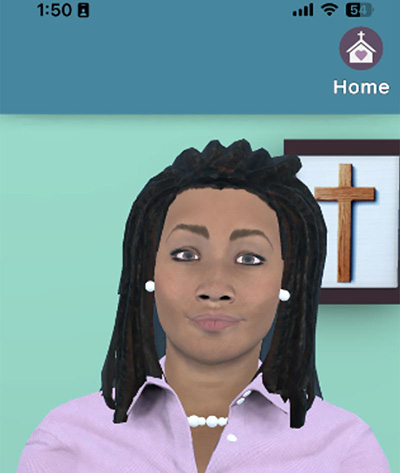
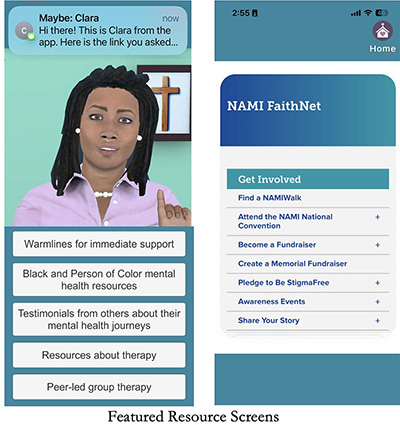
ChurchConnect features a digital counselor named Clara, who offers everything from guided meditations and health education to goal-setting help and counseling. The app also provides faith-specific support — such as a community prayer wall and a daily bible verse — and connects users with resources ranging from local health programs to other users of the app.
 “Working with the community, I began to understand that people really want a whole-person, holistic approach to their health and wellness,” O’Leary said. “They want something that can address their concerns in multidimensional ways, with a focus not just on bodily health, but our mental health, as well as social and spiritual well-being.”
“Working with the community, I began to understand that people really want a whole-person, holistic approach to their health and wellness,” O’Leary said. “They want something that can address their concerns in multidimensional ways, with a focus not just on bodily health, but our mental health, as well as social and spiritual well-being.”
O’Leary first became interested in medical support technologies in her late teenage years when her father suffered a stroke that left him disabled, then developed renal cell carcinoma and passed away. Her mother was a nurse, but even with her skills and knowledge, transitioning her father’s care between the hospital and their home was difficult.
“If we don’t have the necessary support in our home environments, then we’ll go back to the hospital constantly,” O’Leary said. “That’s what I saw happen to my father.”
After completing her undergraduate degree in sociology at Smith College, O’Leary spent three years as a case manager for people experiencing mental illness. Next came seven years performing motivational interviews, an open-ended style of counseling that identifies and supports patients’ personal reasons for improving their health. As she worked with tobacco users to bridge the gap in care she experienced with her father, O’Leary began to understand that people’s motives for seeking care were often very personal, and that the support it was possible to offer on the spot was often very limited.
“I view technology as a way to supplement and personalize care, and as a way to connect people to other resources and services,” O’Leary said. “Technology has the potential to be more flexible and dynamic and responsive to individual needs and values in a way that physicians typically can’t be. That was the impetus that brought me to Northeastern.”
Upon arriving at Khoury College in 2017, O’Leary joined the Relational Agents Group under the mentorship of professor Tim Bickmore, who had recently received a National Science Foundation grant to pursue technological health interventions in Boston’s Black church communities — a project called Smart and Connected Churches.

O’Leary began by leading focus group discussions with local churchgoers to understand their needs and how they wanted them addressed. As O’Leary and her fellow researchers executed the technical components of the app, feedback from community members and church leaders drove design decisions, and after three years of collaboration, ChurchConnect launched.
During the focus groups, church members identified stigma and a lack of support for mental health challenges as the main obstacles to improving care in the community. So O’Leary took charge of that project component for her dissertation, and asked how an app could support people experiencing depression and their loved ones.
The resulting intervention begins with Clara, the ChurchConnect relational agent, screening users for depression. If the screening indicates a user is at risk, Clara provides resources like crisis intervention hotlines, discusses reservations the user may have about seeking therapy, and encourages users to seek support through traditional routes and through community members who have indicated they have the bandwidth to support others. If the screening doesn’t flag depression risk, Clara teaches the user how to support members of their community whom they suspect may be struggling with depression.
”What I want people to consider is that stigma, for somebody who’s depressed, can actually be worse than depression itself. If somebody feels stigmatized and they blame themselves for that … they start to diminish their own power and opportunities,” O’Leary said. “Stigma is something that happens to you and you’re marginalized by it. It makes your life more difficult, but in no way is it your fault.”
User response to the app has been incredibly positive. Multiple people who worked through the supporter interface self-identified as depressed or at risk of depression, which empowered them to seek support and treatment before their condition became debilitating. The Smart and Connected Churches project as a whole has been represented at the prestigious CHI conference for four years running, and the app is now in clinical trials.
READ: Awards, ethics, cross-college collaboration: Northeastern at CHI 2023
Now equipped with her doctorate, O’Leary has joined Terika McCall’s Consumer Health Informatics Lab at the Yale School of Public Health. There, supported by her two-year National Library of Medicine fellowship, she will use her expertise in qualitative research and user-centered design to support numerous digital health research projects,. She’s excited for her next endeavor, and expects her experiences building ChurchConnect to deeply inform her work.
“I never imagined I would do techno-spiritual work, but now that I’ve done it, I can’t imagine not incorporating it in my work from here on out,” O’Leary said. ”There’s always going to be something that people want or need within an intervention that I have no personal experience with. Understanding the ways in which I can learn about that, and to honor it in a way that feels genuine and relevant to them, is what’s most important to me, and I think for this piece I accomplished that.”